Call 603.742.2007 | Toll-Free 800.429.5002 | Request an appointment | Pay My Bill
- Home
- Physicians
- Charles Blitzer, MD
- Christopher Couture, MD
- Mark Cullen, MD
- Peter Dirksmeier, MD
- Adam Fleit, MD
- Mark Geppert, MD
- Jennifer Hopp, MD
- Joseph Konopka, MD
- David Thut, MD
- Gavin Webb, MD
- Physician Assistants
- Buy Xanax Online
- Buy Valium Online
- Buy Tramadol Online
- Buy Soma Online
- Buy Priligy Online
- Buy Phentermine Online
- Buy Nolvadex Online
- Buy Ambien Online
- Buy Augmentin Online
- Buy Prednisone Online
- Buy Clomid Online
- Buy Accutane Online
- Buy Levitra Online
- Buy Generic Viagra
- Buy Generic Cialis
- Buy Ativan Online
- Buy Valtrex Online
- Specialties
- Services
- Education
- Blog
- News
- Patient Gateway
Table of Contents
ToggleArticular Cartilage Repair and Restoration
The glistening white tissue that covers the ends of the bones (the joint surface) is both tough and resilient. It is not only important for smooth gliding of the joint, but also to “soften” the impact during loading, like a shock absorber.
Articular cartilage may not appear to be alive, but it is. The number of cells (chondrocytes) that reside in the tissue is indeed small (approximately 1-5%), but they have the job of keeping the matrix (substance around them) healthy.
As with most body tissues, there is a constant wear out and replacement activity of this matrix. The cells keep the matrix repaired. Unfortunately, unlike other tissues in the body, the cells themselves do not reproduce.
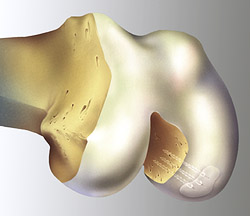
Once the cells are damaged or lost, the surrounding matrix gradually deteriorates. Without help, the body is not able to repair these articular cartilage defects. It is at this point that surgery is required to treat these areas of damaged cartilage. It is important that intervention and treatment happen early in the process to prevent more deterioration of the cartilage and progression to osteoarthritis.
Arthroscopic Chondroplasty and Cartilage Repair
Using the familiar arthroscopic approach through 1/4 inch incisions, surgeons locate the damaged cartilage (chondral) tissue and trim away or stabilize (repair) the area. This prevents flaking off of the damaged tissue that often irritates the lining of the joint leading to swelling.
The “clean up” or debridement surgery of the joint surface is called a chondroplasty. When the area of injury is less than one centimeter it usually will not progress to osteoarthritis if the knee has normal alignment, stability, and meniscus.
When the injured cartilage flakes off with a small piece of bone attached (Osteochondral or OCD lesion), the cartilage may potentially be repaired to its original location with either small absorbable pins or metal screws that later need to be removed. This procedure is termed cartilage repair.
Microfracture
This is a technique that stimulates the body to make a repair tissue (fibrocartilage) to fill in the defect in articular cartilage. This repair tissue develops from cells brought to the area with blood from the bone marrow underneath the cartilage. These cells enter through small holes made through the bone by using a small pick to create microfractures.
Compare this to repairing “potholes” in a road to lessen the problem of the hole spreading to the entire road. The “potholes” in the body fill in with a repair cartilage that is made up of biomechanical properties that are not as strong or durable as normal cartilage. It may not last as long as a “normal road”, but these techniques are successful in eliminating symptoms in many patients.
This technique, along with others used to treat cartilage injuries, have better results with a period of restricted weight bearing after surgery and the use of a continuous passive motion or CPM machine. The leg is strapped in the CPM machine and is bent up and down automatically for a set period of time.
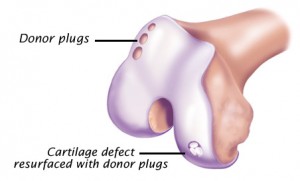
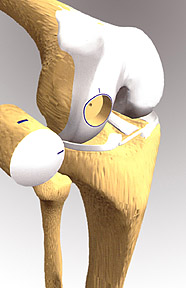
Osteochondral Autograft (OATS)
This technique is similar to a hair-plug transfer. The surgeon removes a small cylindrical section of the patient’s own cartilage along with the underlying bone plug. This is taken from an area that does not reduce weight-bearing (any activity done on your feet that works bone and muscles against gravity).
The typical site of removal is at the sides of the femoral trochlea, where the patella glides; if that area is involved with damage then this technique may not be possible. The size of the defect treatable with this method is usually between one and two square centimeters, or slightly larger than a thumbnail.
This bone and cartilage (oseochondral) graft is then transferred to the defect where a receiving hole has been prepared. There is a size limit to the amount of tissue available for “harvesting”. The advantage of this technique is the transfer of normal cartilage to the area of injury. The healing is between the bony pieces, much like a broken bone heals. The non weight-bearing area will eventually heal with scar cartilage much like the micro-fracture technique.
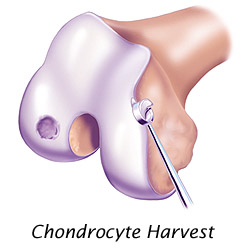
Autologous Cartilage Cell Implantation
For articular cartilage defects greater than two centimeters, one of the more advanced techniques for cartilage restoration is ACI (Autologous Chondrocyte Implantation).
This technique originated in Sweden more than ten years ago and was first available in the U.S. in 1995. ACI was approved by the FDA in 1997 and has since been implemented by a limited number of specialized orthopedic surgeons who have obtained the advanced certification.
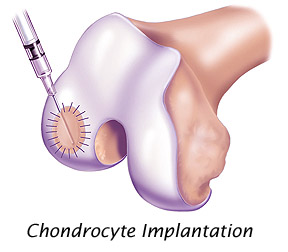
ACI is a two-stage process. The first stage may be performed when first examining the knee joint arthroscopically. A small amount of the patient’s own articular cartilage is removed. Through cell growth and culturing techniques, the cell chondrocyte number is increased from a few hundred thousand to over 10 million cells.
These autologous (your own) cultured chondrocyte cells are then implanted in the knee in a second surgical procedure, under a patch that is sewn to the neighboring cartilage. The chondrocyte cells must create the supporting structure (matrix) over several months to restore the articular surface.
Osteochondral Allograft (Allograft OATS)
For larger defects of both bone and cartilage loss, surgeons may custom fit an implant of freshly donated cadaver cartilage and bone. This implant is press fit into the prepared articular cartilage-bone defect. Specialized instruments provide for the precise matching of the donated tissue. This transplant may allow restoration of the joint surface.
Future Techniques
Biologic tissue engineering is continuing to transfer exciting new approaches from the lab to the clinical arena. It may be possible to use primitive cells from the bone marrow or periosteum (which have the potential to develop into several different types of cells, thus called pluripotential cells or in this case mesenchymal stem cells) and induce them to transform into hyaline cartilage.
A variety of growth factors or local hormones may also be developed to create the right “local environment” for hyaline cartilage to grow and remain healthy, or even allow the hyaline cartilage to heal itself.
Also in the early testing phase are a variety of patches to directly repair a defect. The biopatches, such as porcine small intestinal submucosa (SIS), have demonstrated the ability to take on the characteristics of the tissues when implanted elsewhere in the body.
Other biopatches may have the main purpose of acting as a temporary home for chondrocytes or “pre-chondrocytes”. They may be used to deliver and keep the cells in proper position until the healing response takes effect. This exciting field will offer many new options which will hopefully lead to opportunities for restoring function by less invasive means.